Polypharmacy: perhaps it hurts, but it will never go away
Almost half of 9300 Mediately app users (47% precisely) who participated in this year’s Digital Doctor Survey, said their average patient is taking at least 5 drugs. Surprised? I believe not. Polypharmacy is a widespread and overwhelming phenomenon. However, answers to Digital Doctor questions about polypharmacy revealed many new aspects. A bit of a surprising fact: on the topic of polypharmacy being either an offensive or defensive type of medical practice, Mediately doctors in our survey were almost tied, with 48% declaring it an offensive and 52% a defensive type of medical practice. They are practically divided in half!
Digital Doctor by Mediately is one of the biggest European surveys among doctors
We polled doctors in 12 countries where the Mediately app is currently present. It was interesting to see how different their viewpoints on polypharmacy were – especially since they were more or less united on other topics, such as sources of medical knowledge and work satisfaction. This leads to the thought that practicing medicine is more about personal characteristics and cultural differences than most of us would be likely to admit. Nevertheless, there was one common feature: if a medication is the physician's only weapon, they will use it. No doubt.
The term polypharmacy is not uniformly defined, but it generally means taking several different medications at the same time on a regular basis, usually 5 or more. Decades ago, polypharmacy was when physicians prescribed mixed drugs on one prescription. Today, the term polypharmacy is most commonly associated with a higher risk of adverse events and drug interactions.
Let’s say straightforward: polypharmacy will never go away, even if it hurts sometimes. If 47% of polled physicians say their average patient is taking more than 5 medications, they nailed it. You might hear that sounds negative, but it's a fact. And besides all: polypharmacy might be a bad thing only if the medications serve no purpose or cause more harm than good. This “pain” might be your new reality, but it doesn’t need to hurt so much.
“We have to distinguish between polypharmacy, which I believe is needed, from polypharmacy, which is a result of not paying attention to individual needs,” professor Stefano del Prato, the world's well-known expert in endocrinology and metabolism, said in our interview. He believes that we always have to consider our treatment goals and many specific characteristics like age, people’s life habits, and life expectancy. “Some decades ago, the mantra was to intensify treatment, try to treat all different conditions, but now we also have to consider the right balance between risks and benefits,” he is convinced.
Physicians know that polypharmacy often happens when a person has many chronic diseases, such as diabetes, high blood pressure, high lipids, heart failure, cardiovascular disease, osteoporosis, and symptoms such as pain or insomnia, requiring long-term treatment with medications. Chronic diseases and symptoms accumulate with age; for this reason, especially older adults are at higher risk of polypharmacy. Mediately Digital Doctor polled physicians also indicated that the age of the population is the main reason behind polypharmacy (62%). The interesting fact was that 41% of polled doctors also declared insufficient awareness of potential harms as the reason for polypharmacy.
In clinical terms, polypharmacy contributes to an increased risk of adverse drug events and drug-drug interactions, as well as decreased medication adherence. Occasionally associated with adverse patient outcomes and even hospitalizations, polypharmacy is commonly considered something to be avoided. There is evidence that polypharmacy is potentially associated with inappropriate prescribing. However, more recent research has shown that appropriately managing patients with targeted medications can prevent unplanned hospital admissions.
Hence clinicians need to differentiate between two types of polypharmacy: appropriate polypharmacy (when all medicines are prescribed to achieve the specific therapeutic objective and medication therapy has been optimized to prevent adverse drug reactions) and inappropriate polypharmacy (when one or more medications are prescribed than clinically indicated, resulting in adverse patient outcomes and not achieving the therapeutic objective).
One study clearly showed that we cannot assume that polypharmacy is always harmful and that the clinical reasoning by which medicines have been prescribed needs to be considered. The goal should be for the patients to only receive the appropriate and targeted drug therapy.
What do you think are the main reasons behind polypharmacy (using five or more medications simultaneously)?
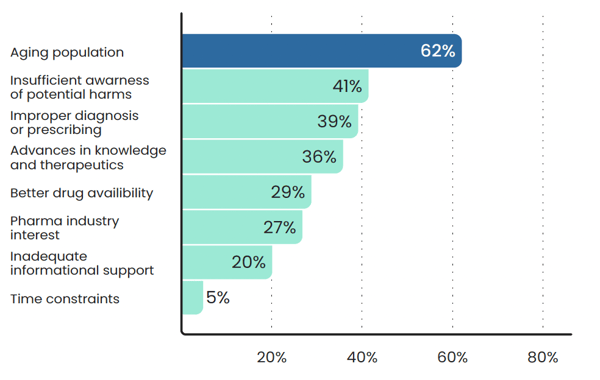
Source: Digital Doctor, a survey conducted by Mediately, 2023
Clearly, we are not performing surveys to spend physicians’ time. We use the data to find out how to help them, what their unmet needs are and try to make their clinical work easier and save them time. At the end of 2023, our Interaction Checker was released in the Mediately application. It is our answer to the unmet needs of our users, doctors.
Mediately Interaction Checker is an important feature that can help doctors avoid potential adverse consequences of the inevitable appropriate polypharmacy. What about other strategies to prevent polypharmacy, especially among the elderly? We have collected some for you:
- Maintain an accurate list of medications and medical history and update regularly.
- Encourage patients to bring/tell/list all medications, including prescription, OTC, supplements, and herbal preparations.
- Review any changes with the patient and caregiver.
- Use the simplest possible dosing regimen, the lowest number of medications.
- Try to link each prescribed medication with its diagnosis.
- Review therapy regularly to consider all possible unnecessary medications.
- Screen for drug-drug and drug-disease interactions.
- When possible, use a team approach, involving the caregiver or family and pharmacist (community pharmacist).
- Avoid starting potentially harmful medications; use AGS Beers Criteria.
- Start a new medication at the lowest dose and then titrate slowly whenever possible.
- Avoid starting medications to combat the potential side effects of other medications.
During transitions of care exercise careful medication reconciliation with proper communication handover.
Co-author: Rok Ješe
Sources:
- Hughes C. Appropriate and inappropriate polypharmacy- Choosing the right strategy. Br J Clin Pharmacol. 2021 Jan;87(1):84-86.
- Lavan AH, Gallagher P. Predicting risk of adverse drug reactions in older adults. Ther Adv Drug Saf. 2016 Feb;7(1):11-22.
- American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults; Journal of the American Geriatrics Society.


